Effective Ways to Read an EKG for Better Cardiovascular Health in 2025
Understanding how to read an ECG is essential for anyone involved in healthcare, particularly in cardiology. As cardiovascular diseases continue to rise, mastering **ECG interpretation** is vital for early detection and effective management of heart conditions. In this article, we will explore various aspects of **ECG reading**, including the basics of electrocardiogram analysis, rhythm identification, and the significance of different waveforms. Whether you’re a beginner or a seasoned healthcare professional, this comprehensive ECG reading guide will enhance your skills and knowledge in cardiac health assessment.
Understanding ECG Basics
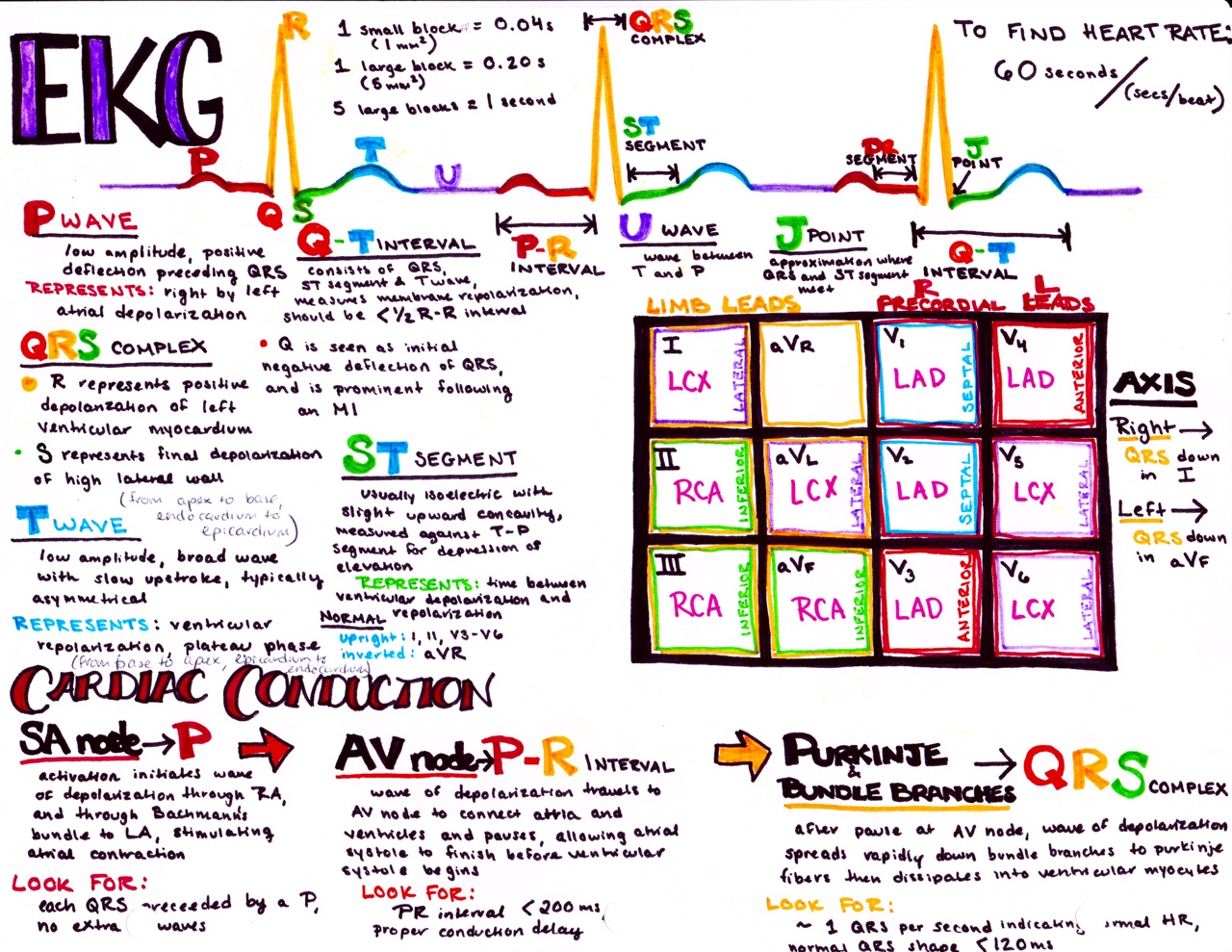
The **ECG basics** begin with understanding what an electrocardiogram measures. An ECG captures the electrical activity of the heart, illustrated through waveforms that represent cardiac cycles: the P wave, QRS complex, and T wave. Mastery of ECG reading requires knowledge of the **heart conduction system** and the ability to recognize normal and abnormal ECG patterns. The normal heart beats with electrical impulses that cause the heart muscle to contract and pump blood. This rhythmic activity generates a wave pattern on the ECG that healthcare professionals analyze to assess a patient’s heart health.
ECG Waveforms: PQRST Waves Explained
The **PQRST waves** are critical components of an ECG waveform. The P wave represents atrial depolarization, while the QRS complex signifies ventricular depolarization. Recognizing these elements is key to understanding heart rhythms. The T wave reflects ventricular repolarization, completing the cycle. Abnormalities in these waveforms can indicate various cardiovascular issues, such as **atrial fibrillation recognition** or **ventricular tachycardia diagnosis**. For example, an inverted T wave may suggest ischemia, whereas a widened QRS complex could indicate underlying conduction disturbances.
Lead Placement Techniques for Accurate ECGs
Proper **lead placement techniques** are crucial for obtaining high-quality ECG readings. Different lead configurations affect the interpretation of heart rhythms, making accurate placement essential. For a 12-lead ECG, positions for limb leads, such as RA (right arm), LA (left arm), RL (right leg), and LL (left leg), are standardized to ensure consistency across readings. Furthermore, chest leads (V1-V6) provide vital information about anterior and lateral heart walls. A well-placed ECG allows for precise **heart rate calculation** and rhythm strip evaluation, which is necessary for detecting abnormalities.
Heart Rate Calculation in ECG Analysis
Calculating heart rate is a crucial part of **ECG interpretation**. This can be done using various methods, such as the 300-method, where you count the number of large boxes between R waves and divide this number into 300. Alternatively, one can use the R-R interval method, which involves measuring the distance between successive R waves and using this value to determine heart rate. Knowing how to analyze heart rate and arrhythmias—from **normal ECG patterns** to **abnormal ECG signs**—deepens your understanding of cardiac cycle phases and how they inform clinical decision-making.
ECG Interpretation Techniques
Effective **ECG interpretation** involves more than just recognizing waveforms. It includes understanding the context of the patient’s history and symptoms. Recognizing patterns associated with different arrhythmias and utilizing **critical care ECG** techniques can significantly impact patient outcomes. Moreover, learning how to interpret 12-lead ECGs versus single leads is essential in varying clinical situations, from stable patients to those requiring emergency care.
Arrhythmia Classification and Recognition
Classifying arrhythmias through **heart rhythm identification** is an essential skill in ECG analysis. Common types include atrial fibrillation, ventricular fibrillation, and supraventricular tachycardia. Each arrhythmia presents unique patterns that can be noted in the **ECG waveform**. For instance, atrial fibrillation is identified by a lack of discrete P waves and an irregular ventricular response, while ventricular tachycardia often presents as a rapid sequence of monomorphic QRS complexes. Utilizing **ECG troubleshooting** techniques can improve diagnostic accuracy and assist in **arrhythmia management**.
ST Segment Abnormalities and Their Implications
Understanding **ST segment abnormalities** is crucial for interpreting evidence of ischemia and myocardial infarction. An elevated ST segment may indicate acute coronary syndromes, which require immediate attention and intervention. The evaluation of this segment, alongside the T wave and QRS complex, helps frame the complete **cardiac cycle understanding**. A thorough analysis of the ST elevation can guide further tests and treatments, making it a critical point in patient monitoring during acute care.
Practical Example: Using ECG for Ischemia Detection
A practical example of leveraging **ECG analysis** in clinical practice involves using the ECG to detect ischemia. Patients presenting with chest pain can undergo an immediate ECG to look for changes in the ST segment, which may suggest reduced blood flow to the heart. For example, if you encounter a patient with chest discomfort and elevated ST changes in leads II, III, and aVF, it can indicate an inferior wall ST elevation myocardial infarction (STEMI). Quick recognition and accurate interpretation can save lives, showcasing the significance of proper **ECG machine operation** in the emergency setting.
Advanced Techniques and Technologies in ECG
As healthcare evolves, advanced technologies in **ECG** practices are essential for effective patient management. Emerging techniques utilizing machine learning and artificial intelligence allow for automated **ECG interpretation** and enhance the accuracy of analyses. Integrating **health informatics** in ECG processing facilitates better data sharing between healthcare providers, eliminating traditional obstacles and improving the speed and quality of cardiovascular assessments.
Real-Time ECG Analysis and Telemedicine Integration
Telemedicine’s evolution allows for addressing cardiovascular health remotely through **real-time ECG analysis**. Patients can undergo **remote ECG monitoring**, enabling healthcare providers to identify arrhythmias or ischemic changes without patients needing to visit a clinic. This approach enhances patient engagement and ensures timely interventions while promoting ongoing **patient education on ECG** relevance. As wearable ECG devices gain popularity, their use in tracking heart health can potentially increase adherence to preventive measures, providing vital insights into **heart condition monitoring**.
NLP in ECG Data Extraction and Interpretation
The use of **natural language processing (NLP)** in cardiology is creating new avenues for ECG data analysis. Techniques in **extracting ECG data** using NLP can automate the reporting process, streamline documentation, and enhance readability of ECG results. This forward-thinking approach enables clinicians to identify heart diseases proactively while managing patient communications effectively, ensuring optimal outcomes. Such innovations stand to revolutionize **ECG training**, significantly aiding healthcare professionals in mastering **ECG interpretation skills**.
Key Takeaways
- Understanding **ECG basics** is crucial for mastering cardiac assessments.
- Proper **lead placement** and accurate **heart rate calculations** facilitate effective analysis.
- Proficiency in recognizing **arrhythmias** can improve patient outcomes.
- Incorporating advanced technologies and **NLP** in ECG processes enhances efficiency.
- Telemedicine’s role in facilitating **patient monitoring** across distances is increasingly significant.
FAQ
1. What are the common **abnormal ECG signs** to watch for?
Common **abnormal ECG signs** include ST segment elevations or depressions, irregular rhythms such as atrial fibrillation, and QRS complex irregularities. Recognizing these signs helps in diagnosing various heart conditions, including ischemia and arrhythmias.
2. How can I improve my **ECG interpretation skills**?
Improving **ECG interpretation skills** can be achieved through practice with **ECG worksheets**, engaging in **ECG training** modules, and participating in hands-on workshops. Continuous education and real-life application also play significant roles in skill enhancement.
3. What should I know about **patient history in ECG** interpretation?
Understanding a patient’s medical history is vital in **ECG interpretation** as it provides context for any abnormalities detected. Factors such as previous heart conditions, medication history, and family history of cardiac diseases can influence ECG results significantly.
4. How does **ECG software** assist in heart condition assessments?
**ECG software** can assist by providing computerized analyses, flagging potential abnormalities, and offering insights into heart rhythm patterns. This technology enhances accuracy, ensures timely diagnosis, and aids in making informed clinical decisions.
5. Why is **telemetry monitoring** important in critical care?
**Telemetry monitoring** allows for continuous observation of patients’ heart rhythms, especially in critical care settings. This real-time ECG data helps identify acute changes in cardiovascular status, ensuring immediate interventions when necessary.
6. What are the advantages of utilizing **wearable devices for ECG monitoring**?
Wearable devices for **ECG monitoring** provide continuous heart activity tracking outside clinical settings, promoting early detection of arrhythmias and facilitating timely healthcare interactions. They empower patients in managing their health more proactively.
7. How can I interpret **ECG artifacts**, and what do they mean?
Interpreting **ECG artifacts** involves recognizing disturbances in the ECG signal caused by patient motion, poor electrode contact, or external interference. Awareness of these artifacts is essential for ensuring accurate ECG readings and minimizing misdiagnosis.